Helping you move pain free in as little as 7 days without surgery!
Dr. Gayan Poovendran, MD offers advanced, non-surgical solutions for joint, ligament, and muscle pain.
No surgery | No medication | Minimal downtime

Dr. Gayan Poovendran, MD offers advanced, non-surgical solutions for joint, ligament, and muscle pain.
No surgery | No medication | Minimal downtime
![]()
Revitalize your body. Renew your game.


![]()
Pro Institute Poovendran Regenerative Orthopedics
Regenerative Sports Medicine Physician & A Private Medical Practice located in Davie, FL
At Pro Institute Poovendran Regenerative Orthopedics, advanced healing science combines with genuine, personalized patient care to create transformative health outcomes. Founded by the dedicated husband-and-wife team of Dr. Gayan Poovendran and Geetha Poovendran, our South Florida practice specializes in revolutionary treatments that help your body heal naturally.
Through advanced therapies like PRP, stem cell treatments, and innovative peptide protocols, we’re transforming how patients approach healing and recovery. At Pro Institute, you’re not just another patient – you’re part of our extended family, receiving personalized care that addresses your unique needs and goals.
Our Mission
Dr. Gayan Poovendran and Geetha Poovendran built Pro Institute Poovendran Regenerative Orthopedics on a foundation of ethical, honest, and transparent care. Our mission centers on putting your well-being at the heart of everything we do, embracing a family-first mindset that treats every patient with the same compassion and respect we’d offer our own loved ones. We believe in empowering you with knowledge, taking time to explain your condition and treatment options in clear, understandable terms.
Through our comprehensive approach combining regenerative therapies, advanced technologies, and holistic treatments, we help you achieve optimal health and performance. At Pro Institute, we’re committed to providing minimally invasive solutions that support your body’s natural healing processes while maintaining the highest standards of medical excellence.
Understanding How Stem Cell Therapy Works for Your Recovery
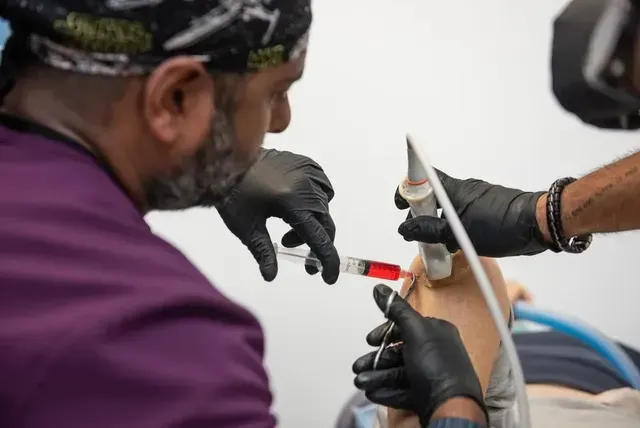
Stem cell therapy represents a breakthrough approach to healing that harnesses your body’s natural regenerative power. At Pro Institute Poovendran Regenerative Orthopedics, we extract stem cells from your own adipose tissue and bone marrow to create concentrated healing solutions. This advanced treatment stimulates new cell generation while supporting your body’s inherent ability to repair damaged tissues.
Why Stem Cell Therapy Delivers Superior Healing Results
Your body contains powerful regenerative cells that can transform how you recover from musculoskeletal injuries. Pro Institute specialists concentrate these cells to create potent healing formulations that accelerate tissue repair. We administer multiple injections per treatment area to optimize therapeutic outcomes and promote comprehensive healing.
- Reduces inflammation naturally without synthetic medications
- Stimulates growth of healthy new tissue in damaged areas
- Accelerates recovery time compared to traditional treatments
- Minimizes scar tissue formation during healing process
- Provides long-lasting pain relief through tissue regeneration
Addressing Common Injuries Through Advanced Cellular Medicine
Many patients struggle with chronic pain from sports injuries, arthritis, and degenerative conditions that limit daily activities. Pro Institute uses stem cell therapy to treat meniscus tears, rotator cuff injuries, hip and knee osteoarthritis, tennis elbow, and hip bursitis effectively. Our comprehensive approach targets the root cause of your discomfort rather than merely masking symptoms.
- Treats multiple injury types in single treatment sessions
- Addresses underlying tissue damage causing chronic pain
- Reduces dependence on pain medications and their side effects
- Improves joint function and mobility over time
- Prevents further deterioration of affected tissues
We prepare you thoroughly for treatment by recommending you avoid aspirin and NSAIDs for four days before your appointment. Our Pro Institute team also suggests staying well-hydrated and arranging transportation home after your procedure to ensure optimal safety and comfort throughout your healing journey.
How PRP Transforms Athletic Performance and Recovery Outcomes
PRP injections deliver concentrated platelets directly to injured tissues, creating powerful healing responses that traditional treatments cannot match. These platelets contain essential growth factors that activate your body’s natural repair mechanisms, accelerating recovery from sports injuries and chronic conditions. Our advanced centrifuge technology concentrates your platelets to therapeutic levels, maximizing their regenerative potential for optimal healing results.
Debunking Common PRP Treatment Misconceptions
Many athletes avoid PRP therapy due to widespread myths about pain, effectiveness, and recovery time. Pro Institute Poovendran Regenerative Orthopedics uses ultrasound guidance and hematology analyzers to deliver precise, comfortable treatments that produce measurable results. We charge per treatment area rather than per injection, making this advanced therapy more accessible for patients seeking natural healing solutions.
- PRP treatments cause minimal discomfort with proper ultrasound guidance techniques
- Results typically appear within weeks, not months like many believe
- Treatment works for chronic conditions, not just acute injuries
- Your own blood eliminates risks of allergic reactions or rejection
- Multiple conditions can be treated simultaneously during single sessions
The Evolution of PRP Technology in Modern Medicine
Regenerative medicine has revolutionized how we approach musculoskeletal injuries over the past two decades. Pro Institute has embraced cutting-edge PRP technology that surpasses older methods through precision guidance systems and quality control measures. Our hematology analyzers verify optimal platelet concentrations before each injection, providing transparency and confidence in your treatment process.
- Advanced centrifuge systems create higher platelet concentrations than earlier methods
- Ultrasound and fluoroscopic guidance improve injection accuracy significantly
- Modern PRP kits maintain sterility and potency throughout treatment
- Real-time platelet counting ensures therapeutic dosing for each patient
- Comprehensive evaluations identify ideal candidates through genetic testing capabilities
We customize every PRP treatment plan based on your specific medical history, current diagnosis, and recovery goals. Pro Institute treats conditions ranging from frozen shoulder and tennis elbow to plantar fasciitis and knee arthritis using personalized protocols. Our team prepares you thoroughly by recommending you avoid NSAIDs for four days and arrange transportation home after your appointment to optimize healing and safety.
Preventing Joint Deterioration Through A2M Molecular Therapy
A2M represents cutting-edge molecular therapy that stops harmful enzymes from destroying your joint cartilage before irreversible damage occurs. This naturally occurring protein, produced by your liver, acts as a protective shield around damaged tissues by binding to destructive proteases. We extract and concentrate A2M from your blood using advanced filtration technology that goes beyond standard processing methods, creating powerful therapeutic concentrations for targeted injection therapy.
Maximizing Your Body's Natural Defense Against Joint Breakdown
Your joints face constant attack from proteases that break down cartilage and connective tissues, especially after injury or with age-related wear. Pro Institute harnesses A2M’s remarkable ability to neutralize these harmful enzymes directly at injury sites. Dr. Poovendran uses precise injection techniques to deliver concentrated A2M molecules where they can provide maximum protective benefits for your damaged tissues.
- Comprehensive preparation maximizes treatment effectiveness and safety outcomes
- Targeted enzyme neutralization reduces ongoing tissue damage progression
- Natural protein therapy eliminates synthetic drug side effects and complications
- Advanced filtration creates higher therapeutic concentrations than standard methods
- Direct injection placement optimizes healing responses in specific problem areas
Comparing A2M Treatment to Traditional Joint Therapies
Pro Institute Poovendran Regenerative Orthopedics offers this advanced therapy for conditions including herniated discs, osteoarthritis, torn meniscus, degenerative disc disease, and spinal injuries. Traditional treatments often mask symptoms while joint damage continues, whereas A2M actively protects remaining healthy tissue from further breakdown.
- Longer-lasting results compared to corticosteroid injections that wear off quickly
- Addresses underlying tissue breakdown rather than masking symptoms temporarily
- No risk of cartilage damage associated with repeated steroid use over time
- Compatible with other regenerative therapies for combined therapeutic benefits
- Effective for both spinal and peripheral joint conditions across multiple body systems
We require patients to discontinue anti-inflammatory medications and certain supplements like ginger, fish oil, and turmeric before treatment to optimize A2M effectiveness. Pro Institute conducts comprehensive assessments to identify the precise source of your symptoms, allowing us to craft customized treatment plans that target your specific condition for optimal therapeutic outcomes.
The Future of PRP Hair Restoration Promises Revolutionary Results
PRP hair restoration represents the next generation of non-surgical hair therapy, utilizing your body’s own growth factors to reactivate dormant follicles and stimulate robust new growth. Advanced centrifuge technology separates your blood components to extract concentrated platelets rich in healing proteins that nourish your scalp at the cellular level. This innovative approach transforms how we address hair loss by working with your body’s natural regenerative processes rather than relying on synthetic chemicals or invasive surgical procedures.
Building Long-Term Hair Health Through Sustained Growth Enhancement
Pro Institute Poovendran Regenerative Orthopedics uses specialized techniques that yield true platelet concentrations, evidenced by the distinctive dark coloration that indicates authentic PRP rather than watery plasma substitutes. Our hematology analyzer provides precise platelet counts, ensuring you receive therapeutic concentrations that deliver measurable, long-term results over months and years.
- Strengthens existing hair shafts to resist future breakage and thinning patterns
- Reactivates dormant follicles that have stopped producing visible hair growth
- Improves scalp circulation for sustained nutrient delivery to hair roots
- Creates progressive thickness improvements that compound over multiple sessions
- Provides natural anti-aging benefits for overall scalp health and vitality
Solving Complex Hair Loss Challenges for Both Men and Women
Hair thinning affects people differently based on genetics, stress levels, medical conditions, and hormonal changes that traditional treatments often fail to address comprehensively. Pro Institute specialists evaluate your specific pattern of hair loss to determine if you have alopecia, stress-related thinning, or early-stage balding that responds well to PRP therapy. We customize treatment schedules based on your individual needs, with sessions typically lasting 60-90 minutes and results becoming visible within 6-12 months.
- Addresses multiple types of alopecia through targeted follicle stimulation
- Effectively treats stress-induced hair loss that doesn’t respond to topical treatments
- Works for both male pattern baldness and female hair thinning conditions
- Provides alternatives for patients who cannot use blood thinners during treatment
- Offers early intervention benefits when hair loss is first detected
Proper preparation maximizes your treatment success by eating nutritious meals and staying well-hydrated before your appointment. Pro Institute ensures comfortable experiences through careful scalp numbing and gentle injection techniques that minimize discomfort while delivering concentrated growth factors exactly where your hair follicles need the most support.
Understanding Ozone as a Natural Therapeutic Gas
Ozone therapy harnesses a naturally occurring atmospheric gas to activate your body’s inherent healing mechanisms and defense systems. This reactive oxygen molecule triggers profound physiological responses by optimizing immune function, enhancing cellular oxygenation, and catalyzing the release of beneficial neurotransmitters like serotonin and endorphins. Medical ozone works at the cellular level to combat oxidative stress while strengthening your body’s ability to resist infections, reduce inflammation, and accelerate tissue repair processes.
Transforming Health Outcomes Through Advanced Ozone Applications
Pro Institute delivers ozone therapy through multiple targeted methods, including direct injections for localized healing and intravenous autohemotherapy for systemic benefits. Our specialized combination of ozone with PRP therapy amplifies regenerative effects, creating synergistic healing responses that surpass individual treatment results. This innovative approach addresses complex medical conditions ranging from arthritis pain and sports injuries to chronic fatigue and age-related decline.
- Direct injection delivery targets specific injury sites with concentrated therapeutic effects
- Intravenous autohemotherapy provides comprehensive systemic immune system optimization
- Combined PRP-ozone protocols enhance tissue regeneration beyond standard treatments alone
- Painless treatment sessions deliver measurable improvements within days and weeks
- Cutting-edge technology ensures precise therapeutic gas concentrations for optimal safety
Maximizing Wellness Benefits Through Comprehensive Ozone Treatment
Ozone therapy at Pro Institute Poovendran Regenerative Orthopedics creates wide-ranging health improvements that extend far beyond symptom relief. Patients experience enhanced sports performance, increased energy levels, improved circulation, and stronger antioxidant protection that supports long-term wellness goals.
- Metabolic activation increases cellular energy production and overall vitality levels
- Enhanced immune defense mechanisms provide better protection against harmful microorganisms
- Improved tissue oxygenation accelerates healing and reduces recovery time significantly
- Anti-aging effects promote healthier skin appearance and cognitive function improvements
- Reduced inflammation markers support better joint mobility and pain management outcomes
We prepare patients thoroughly by reviewing current medications, ensuring proper hydration, and conducting comprehensive assessments to customize treatment protocols. Pro Institute combines advanced ozone delivery methods with personalized care plans that address your specific health concerns and wellness objectives for optimal therapeutic results.
Why Shockwave Technology Surpasses Traditional Pain Management Methods
Shockwave therapy delivers targeted high-energy pulses that penetrate deep into damaged tissues, creating healing responses that surface-level treatments cannot achieve. Unlike superficial radial shockwaves used in many clinics, our focal shockwave technology maintains full intensity at depth, reaching calcified deposits near bone structures where conventional therapies fail.
This advanced approach eliminates the need for invasive procedures while providing mechanical stimulation that breaks down damaged tissue and promotes cellular regeneration without pain or incisions.
The Evolution of Shockwave Medicine from Kidney Stones to Musculoskeletal Healing
Pro Institute Poovendran Regenerative Orthopedics has embraced the medical breakthrough that transformed shockwave technology from kidney stone treatment into precise musculoskeletal therapy. Hospital-grade focal shockwave equipment represents decades of technological advancement, delivering concentrated energy that stimulates bone, connective tissue, and muscle regeneration at the cellular level.
- Medical-grade equipment provides consistent energy delivery compared to early shockwave devices
- Ultrasound guidance technology ensures precise targeting of damaged tissue areas
- Advanced focal delivery systems maintain therapeutic intensity throughout tissue depth
- Evidence-based protocols developed through years of clinical research and application
- Integration with regenerative medicine creates comprehensive treatment approaches for complex conditions
Preventing Surgical Interventions Through Proactive Shockwave Treatment
Early shockwave intervention addresses musculoskeletal problems before they progress to surgical candidates, offering patients alternatives to invasive procedures and lengthy recovery periods. Pro Institute uses this technology to treat tennis elbow, golfer’s elbow, calcific tendonitis, jumper’s knee, Morton’s neuroma, plantar fasciitis, and chronic non-healing fractures effectively.
- Non-invasive treatment eliminates surgical risks and extended rehabilitation requirements
- Early intervention prevents chronic pain conditions from becoming treatment-resistant cases
- Mechanical pressure therapy stimulates natural healing without pharmaceutical dependencies
- Quick treatment sessions lasting 5-15 minutes fit easily into busy schedules
- Conditions traditionally requiring PRP injections may respond to shockwave therapy alone
We conduct comprehensive evaluations including symptom assessment, medical history review, and diagnostic imaging to determine your candidacy for shockwave therapy. Pro Institute creates personalized treatment schedules that optimize healing outcomes while minimizing the number of sessions needed to achieve long-lasting pain relief and restored function.
Why Choose Us

![]()
Meet the Doctor
Dr. Gayan Poovendran, founder and medical director of Pro Institute, completed his residency training in family medicine followed by a fellowship in sports medicine at Grant Medical Center in Columbus, Ohio. With dual board certifications from the American Board of Family Medicine and over a decade of experience in regenerative medicine, he brings exceptional expertise to every patient interaction. His background spans working with diverse athletes and serving as team physician for Calvary Christian Academy and Cardinal Gibbons High School in Fort Lauderdale.
Dr. Poovendran is also an active contributor to the medical community, co-authoring articles and serving as a hands-on instructor at regenerative medicine conferences. As both an athlete and weekend warrior himself, he understands the importance of maintaining active lifestyles and approaches each patient with genuine empathy and comprehensive understanding.

Thorne
Thorne sets the quality standards for supplements by being TGA, NSF, and cGMP Certified, and offers over 25 NSF Certified for Sport Products. Confirm Poovendran Regenerative Orthopedic Institute as your HCP Referral during account creation for your ongoing exclusive discount and free shipping.

Pure Encapsulations
Pure Encapsulations® is dedicated to providing nutritional supplements that are designed with integrity using premium ingredients backed by verifiable science, and held to the highest industry standards. Use Code 471998 to purchase your first order!
Pro Institute Is Here to Guide Your Path Forward!
Experience the transformative power of regenerative medicine with treatments designed to support your body’s natural healing capabilities. Our advanced therapies help you recover faster, reduce pain naturally, and return to the activities you love with confidence and improved performance.
Dr. Gayan Poovendran and Geetha Poovendran at Pro Institute Poovendran Regenerative Orthopedics are ready to guide you on your healing journey. Follow us on Facebook and Instagram to learn more about our innovative treatments and patient success stories. Call 305-209-1951 today to schedule your consultation and discover how regenerative medicine can change your life.
![]()
Our Podcast
Davie
Hours Of Operation:
- Monday:
- –
- Tuesday:
- –
- Wednesday:
- –
- Thursday:
- –
- Friday:
- –
- Saturday:
- Closed
- Sunday:
- Closed
FAQs
What conditions do you treat at your practice?
We specialize in treating a wide range of musculoskeletal conditions, sports injuries, and chronic pain issues through regenerative medicine approaches. Our treatments are particularly effective for joint pain, tendon injuries, ligament damage, and various orthopedic conditions that haven’t responded well to traditional therapies. We work with patients aged 14 and older who are seeking alternatives to surgery or long-term medication dependence.
How long have you been providing regenerative medicine treatments?
Dr. Gayan Poovendran has over a decade of experience specifically in regenerative medicine, having practiced in Fort Lauderdale from 2014 to 2021 and Miami Beach from 2021 to 2023 before establishing our current practice. His extensive background includes working with professional athletes and serving as a team physician, giving him deep expertise in advanced treatment protocols. Our practice represents years of refined techniques and proven results in regenerative therapies.
What makes your approach different from other medical practices?
As a family-owned practice, Pro Institute prioritizes building genuine relationships with our patients, taking time to understand your complete health picture before developing treatment plans. Dr. Poovendran avoids medical jargon and ensures you fully understand every aspect of your care, moving at your pace rather than rushing through appointments. We combine advanced regenerative technologies with holistic approaches, offering comprehensive care that addresses root causes rather than just symptoms.
Do you work with physical therapists or other healthcare providers?
Yes, we believe in collaborative care and may recommend physical therapy as part of your comprehensive treatment plan following certain procedures. Dr. Poovendran works closely with other healthcare professionals to ensure you receive well-rounded care that supports your healing and long-term wellness goals. Our integrated approach often includes partnerships with specialists who share our commitment to patient-centered, holistic healthcare.
What should I expect during my first visit to your practice?
Your initial consultation at Pro Institute will be comprehensive and unhurried, with Dr. Poovendran taking time to understand your medical history, current concerns, and personal goals. You can expect a thorough evaluation, clear explanations of your condition, and detailed discussions about all available treatment options without pressure to make immediate decisions. We believe in educating our patients and ensuring you feel comfortable and informed before beginning any treatment protocols.
How do I know if I'm a good candidate for regenerative medicine?
The best way to know if you’re a candidate for cell therapies is to come in for a consultation. We will review any prior imaging studies, as well as conduct a diagnostic ultrasound of the area. The doctor will also review your health history, and determine the best course of treatment.
Am I too old for cell therapies?
Age is NOT a blanket disqualification for prp or stem cell. Factors like overall health and the specific type of therapy are considered more important than age alone. At PRO Institute, we have successfully treated a range of ages, even those well into their 80’s.
Are cell therapies safe?
In fact, the most consistent finding in all cell therapy research is that the procedures are safe with minimal risk.
How much pain will I be in after my procedure?
Some pain is completely normal, and most patients report moderate pain and discomfort at the injection site for 48-72 hours which is typically managed with Tylenol and heating packs. After that, you’ll notice that the pain begins to subside. If the doctor has prescribed any medications, those will help. However, it’s important
to note that anti-inflammatory medications should not be used before or after your procedure. In addition, Dr. Poovendran may also recommend physical therapy.
How do we measure the quality of the cell therapies you're receiving?
At PRO Institute, we utilize a hematology analyzer to measure platelet counts and compare the concentration of platelets before and after centrifugation. This ensures the PRP preparation meets therapeutic dosing thresholds, typically 5 – 15x baseline platelet concentration.
How much do regenerative procedures cost?
The cost of regenerative medicine varies based on the specific treatment and the individual condition being addressed. Because each patient’s needs are unique, our treatment plans are fully customized to ensure the best possible outcomes. As a general guideline, platelet-rich plasma (PRP) treatments typically start at $3,000, while stem cell therapies may begin around $8,000.
Why is the price so high? I've noticed it's available for less elsewhere.
The short answer to that is that you get what you pay for. Our orthobiologic treatments are customized for each individual patient. And with our PRO-formance and A2M PRP procedures, we include ultrasound-guided injections targeting multiple structures within and around the joint, ensuring patients receive the most comprehensive care. The platelet concentration is customized (typically 5x–15x baseline), with platelet count analysis to ensure precision. “Cheaper” prp’s at other places can’t say the same.
Will my insurance company cover prp or stem cell injections?
Currently, most major insurance companies do not cover orthobiologics, like prp or stem cell injections. However, we do offer clear pricing and financing options through CareCredit.
Do you offer any financing?
We do! We offer payment plans through CareCredit. Once CareCredit has approved your application and payment has been received, we can get your procedure scheduled.
Why did the doctor recommend physical therapy after my procedure?
Physical therapy after a PRP or stem cell procedure supports and enhances the body’s natural healing process by restoring mobility, reducing pain, and improving strength. It helps prevent stiffness and re-injury through guided, progressive exercises tailored to your condition. By improving blood flow and reinforcing proper movement patterns, PT maximizes the long-term success of the regenerative treatment. Together, these therapies promote faster, safer recovery and better overall function.